#TeamVaccines
Anish's Story
Research Team Leader
I’m Anish and I work as a Research Team Leader in the Netherlands. Throughout my career, I’ve been fascinated with how medicines work.
For many years, I’ve worked in the world of vaccines. My team focuses on ‘adjuvants’; the part of vaccines which enhances the body’s immune response, which improves vaccine efficacy and is especially important for people with weaker immune systems. Helping to develop effective vaccines is crucial to address emerging global health threats, including the threat posed by AMR, or antimicrobial resistance, now considered as one of the leading public health threats of the 21st century [1].

What is AMR and why is it a problem?
Antimicrobial resistance (AMR) happens naturally when bacteria change and become resistant to everyday antibiotics. The more we use antibiotics, the faster bacteria develop resistance, the less effective antibiotics become and the more likely that bacteria will become ‘superbugs’ (i.e., resistant bacteria that cause fast spreading infections that don’t respond to antibiotics). It’s a dangerous, vicious cycle that puts all of us at risk.. Thus, using antibiotics only when medically necessary is key in delaying the development of resistant bacteria.
AMR by definition makes it harder and sometimes even impossible to treat infections caused by resistant bacteria. Because it doesn’t respond well to existing antibiotics, infections can become life threatening or fatal. By 2050, it’s estimated AMR could cause around 10 million deaths every year. Efforts to develop new generation antibiotics are ongoing, but success is limited, and new antibiotics will also be subject to the development of resistant bacteria overtime [2].
How can vaccines help slow AMR?
AMR happens naturally over time, so we’ll never be able to fully stop it. But vaccines can help – both directly and indirectly. Firstly, they can help slow the impact of AMR directly by protecting people from certain bacterial infections, thus avoiding antibiotic treatment and slowing the emergence of resistant bacteria. Secondly, vaccines prevent viral infections like the flu for which antibiotics are often wrongly used, and thus indirectly decrease antibiotic use and AMR. In addition, by preventing diseases like the flu that are associated with secondary bacterial infections (e.g. strep throat), vaccines avoid treatment with antibiotics that would otherwise contribute to the development of AMR bacteria.
What’s next for vaccines and AMR?
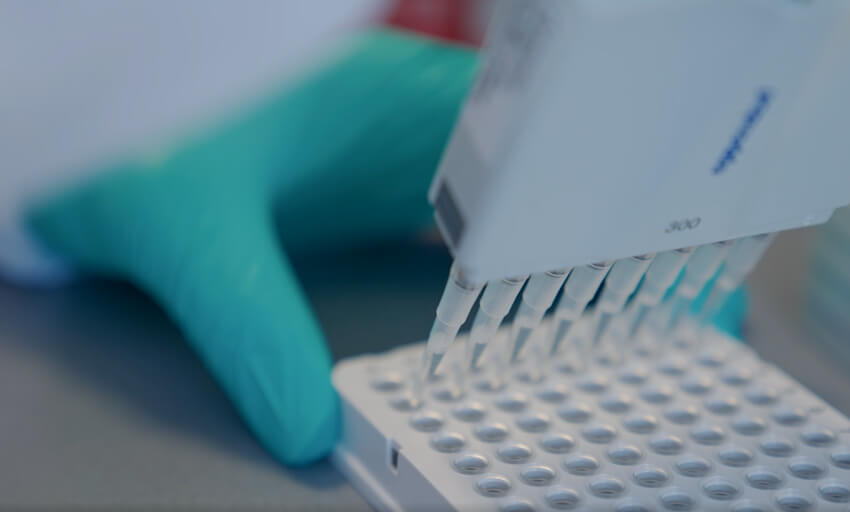
Most vaccines work against viruses, but my team and I are working on new vaccines to protect against infection-causing bacteria, helping to keep more people safe when their immune systems are vulnerable and directly addressing AMR.
Vaccine innovation is only possible through dedication to science, sustained investment and continued collaboration with research and development partners. New vaccines will help protect more people from emerging health threats – like the work scientists across the world are doing for AMR.
This kind of vaccine innovation is a huge global effort and it’s unquestionably something that benefits the whole world. Vaccines alone won’t stop AMR, but they are an important tool in the fight against it because they can help safeguard communities and reduce the spread of infections to others [3]. I’m so proud to help reduce the impact of AMR. It's my hope that we’ll continue to invest in new vaccines to help us reduce AMR and manage and respond to future health crises.
Helping to slow anti-microbial resistance
Vaccines